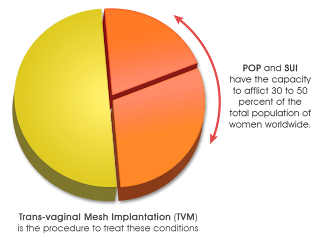
Women searching for the best treatment against incontinence symptoms or bladder weakness probably already have an idea about surgical devices such as the
four types of surgical mesh, medical industry publications report. These are predominantly used as implantable substructures intended to lift the sinking bladder or pelvic floor.
Since bladder control problems are seen mostly in the elderly, most women in their 20s do not often concern themselves about pelvic floor health. Even women who regularly attend yoga classes or Pilates sessions often only regard pelvic exercises as part of their weight-loss and flexibility program. One may also reap these benefits from pelvic exercises. However, most importantly, these types of exercise routines are useful in building stronger and more functional pelvic muscles. Women in their younger years do not often realize how valuable it is to prepare their pelvic muscles for future stresses like vaginal delivery, bone degradation, hormonal inconstancies, hysterectomies, and many more. Oftentimes, women only start noticing the need to strengthen their pelvic musculature after they have delivered their first baby.
For the first few days after a vaginal birth, women may find it hard to tell if they are having leaks, especially if the pain brought by possible vaginal tears or episiotomy are severe enough to cloud the patient’s mind. Moreover, because vaginal bleeding is still active until the fourth day postpartum, it may mask the presence of leak episodes.
Based on a study conducted by clinical researchers in Australia, more than 80 percent of women participants (who have never been pregnant) were seen to have signs of incontinence, and 10 percent of them were later diagnosed with it. Experts consider it to be primarily caused by hereditary factors, erroneous voiding habits, innate tissue problems, or the presence of underlying diseases.
Incontinence often sends out subtle warnings during a woman’s younger years. Unexpected leaks due to excitement or fear often suggest weak bladder control. Other possible incontinence flags include frequent trips to the bathroom, sudden urge to void again even when one had just done so, nocturia (waking up more than two times at night because of a full bladder), and even the feeling of wanting to urinate when the abdomen is slightly pressed.
Lately, as was revealed in a study, health organizations and medical experts worldwide are expecting the rise of urinary tract problems in over 50 percent of people aged 20 years and above by the year 2018. Women turning to modern and untried medical implants may further increase and add up to the already rising vaginal mesh proceedings.
Click here for more information about pelvic floor health.
References:
fda.gov/medicaldevices/safety/alertsandnotices/publichealthnotifications/ucm061976.htm
nursingtimes.net/home/clinical-specialisms/continence/half-of-adults-to-suffer-urinary-tract-symptoms-by-2018/5035678.article
abc.net.au/health/thepulse/stories/2011/11/17/3367126.htm